Embarking on a case study about liver cirrhosis, this exploration delves into the complexities of this chronic liver disease. Cirrhosis, characterized by scarring and inflammation of the liver, poses significant health challenges, and this study aims to shed light on its causes, manifestations, and management strategies.
As we delve deeper into the intricacies of liver cirrhosis, we will uncover the underlying mechanisms that drive its progression, the diverse array of risk factors that contribute to its development, and the clinical signs and symptoms that manifest as the disease takes hold.
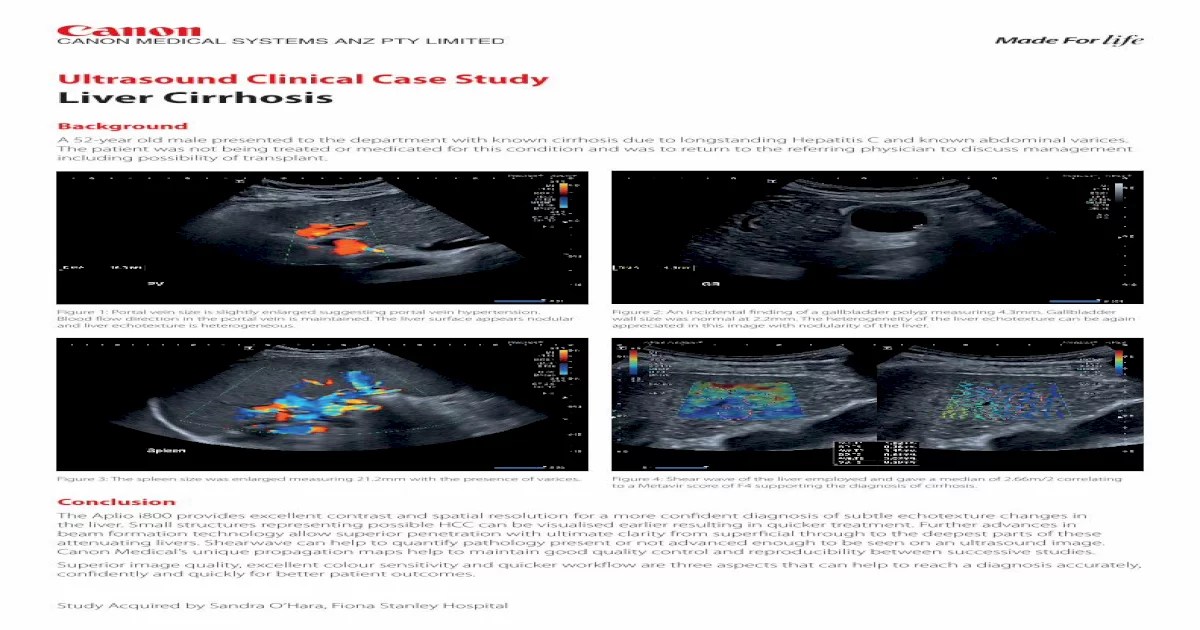
Introduction
The purpose of this case study is to explore the complexities of liver cirrhosis, a chronic and potentially life-threatening condition that affects the liver. Liver cirrhosis is characterized by the scarring and hardening of the liver tissue, which can impair its function and lead to a range of health problems.
Cirrhosis is a serious condition that requires prompt medical attention. Understanding the causes, symptoms, and treatment options for liver cirrhosis is crucial for managing the condition effectively and improving patient outcomes.
Causes of Liver Cirrhosis
There are several factors that can contribute to the development of liver cirrhosis, including:
- Alcohol abuse:Excessive alcohol consumption is a major cause of liver cirrhosis. Alcohol damages liver cells, leading to inflammation and scarring.
- Chronic hepatitis:Viral hepatitis, such as hepatitis B and hepatitis C, can cause chronic inflammation and damage to the liver, leading to cirrhosis.
- Non-alcoholic fatty liver disease (NAFLD):This condition, characterized by the accumulation of fat in the liver, can progress to cirrhosis if left untreated.
- Autoimmune diseases:Certain autoimmune diseases, such as autoimmune hepatitis, can attack the liver cells, leading to inflammation and scarring.
- Genetic disorders:Some genetic disorders, such as hemochromatosis and Wilson’s disease, can lead to the accumulation of iron or copper in the liver, causing damage and cirrhosis.
Pathophysiology
Liver cirrhosis, characterized by the irreversible scarring of liver tissue, is a complex process involving chronic inflammation, fibrosis, and regeneration. Understanding these mechanisms is crucial for managing and preventing this debilitating condition.
Inflammation
Liver cirrhosis often originates from chronic liver injury caused by various factors such as alcohol abuse, viral hepatitis, or autoimmune disorders. This injury triggers an inflammatory response, where immune cells infiltrate the liver and release pro-inflammatory cytokines. The sustained inflammation leads to the activation of hepatic stellate cells, which play a central role in the progression of liver cirrhosis.
Fibrosis
Hepatic stellate cells, once activated, transform into myofibroblasts and begin to produce excessive amounts of extracellular matrix (ECM) components, primarily collagen. This excessive ECM deposition leads to the formation of fibrous bands, which gradually replace healthy liver tissue. The accumulation of scar tissue disrupts the liver’s normal architecture, impairing its function and leading to cirrhosis.
Regeneration
Despite the ongoing inflammation and fibrosis, the liver has a remarkable capacity to regenerate. In response to liver injury, hepatocytes (liver cells) undergo cell division to replace damaged cells. However, in cirrhosis, the regenerative process is often impaired due to the presence of scar tissue and ongoing inflammation.
This impaired regeneration contributes to the progressive loss of liver function and the development of complications associated with cirrhosis.
Causes and Risk Factors
Liver cirrhosis is the end-stage result of chronic liver disease, characterized by the replacement of healthy liver tissue with scar tissue. This irreversible damage can be caused by various factors, and understanding the causes and risk factors associated with cirrhosis is crucial for prevention and early intervention.
The most common causes of liver cirrhosis include:
- Alcohol abuse:Excessive alcohol consumption over a prolonged period can lead to alcoholic liver disease, which can progress to cirrhosis.
- Viral hepatitis:Hepatitis B and C viruses are the leading causes of viral hepatitis, which can cause chronic liver inflammation and lead to cirrhosis.
- Autoimmune disorders:Autoimmune disorders, such as autoimmune hepatitis, cause the body’s immune system to attack the liver, leading to chronic inflammation and cirrhosis.
- Non-alcoholic fatty liver disease (NAFLD):This condition, often associated with obesity and diabetes, involves the accumulation of fat in the liver, which can lead to inflammation and cirrhosis.
Risk Factors
In addition to the primary causes, certain risk factors can increase the likelihood of developing liver cirrhosis:
- Age:The risk of cirrhosis increases with age as the liver’s ability to regenerate diminishes.
- Gender:Men are more likely to develop cirrhosis than women, due to higher rates of alcohol consumption and viral hepatitis.
- Genetic predisposition:Some individuals have a genetic predisposition to liver disease, making them more susceptible to cirrhosis.
- Obesity:Obesity increases the risk of NAFLD, which can progress to cirrhosis.
- Diabetes:Diabetes is a major risk factor for NAFLD and cirrhosis.
- Exposure to toxins:Exposure to certain toxins, such as industrial chemicals or medications, can damage the liver and increase the risk of cirrhosis.
Clinical Manifestations
Liver cirrhosis is characterized by a constellation of clinical signs and symptoms that reflect the progressive damage and dysfunction of the liver. These manifestations provide valuable insights into the severity and extent of the disease.
The most common clinical manifestations of liver cirrhosis include jaundice, ascites, and encephalopathy.
Jaundice
Jaundice, a yellowish discoloration of the skin and whites of the eyes, is a hallmark of liver cirrhosis. It results from the accumulation of bilirubin, a breakdown product of heme, in the blood due to impaired liver function. The severity of jaundice can range from mild to severe and correlates with the degree of liver damage.
Ascites
Ascites, the abnormal accumulation of fluid in the peritoneal cavity, is another common manifestation of liver cirrhosis. It occurs due to a combination of factors, including portal hypertension (increased pressure in the portal vein), reduced plasma protein synthesis, and sodium retention.
Ascites can cause abdominal distension, discomfort, and difficulty breathing.
Encephalopathy
Hepatic encephalopathy is a serious complication of liver cirrhosis that occurs when the liver fails to adequately remove toxins from the blood. These toxins accumulate in the brain, leading to a range of neurological symptoms, including confusion, disorientation, and impaired consciousness.
Encephalopathy is a life-threatening condition that requires prompt medical attention.
Management: Case Study About Liver Cirrhosis
The management of liver cirrhosis aims to prevent further liver damage, control complications, and improve overall well-being. Treatment options vary depending on the stage and severity of the disease, as well as the patient’s overall health and preferences.
The goals of treatment include reducing inflammation and scarring of the liver, preventing and managing complications such as fluid retention, bleeding, and encephalopathy, and improving liver function and quality of life.
Medications
- Antiviral medications:For patients with hepatitis B or C, antiviral medications can help suppress the virus and slow down liver damage.
- Corticosteroids:In some cases, corticosteroids may be used to reduce inflammation in the liver.
- Diuretics:Diuretics help remove excess fluid from the body, which can help reduce swelling and fluid retention.
- Lactulose:Lactulose is a laxative that helps remove toxins from the blood and prevent encephalopathy.
Lifestyle Modifications
- Alcohol abstinence:Abstaining from alcohol is crucial for preventing further liver damage and improving liver function.
- Healthy diet:A healthy diet low in sodium, saturated fat, and cholesterol can help reduce fluid retention and improve liver function.
- Exercise:Regular exercise can help improve overall health and well-being, but it’s important to consult with a doctor before starting an exercise program.
Surgical Interventions
- Liver transplantation:In severe cases of liver cirrhosis, a liver transplant may be necessary to replace the damaged liver with a healthy one.
- Transjugular intrahepatic portosystemic shunt (TIPS):TIPS is a procedure that creates a new connection between the portal vein and the hepatic vein, which can help reduce pressure in the portal vein and prevent complications such as fluid retention and bleeding.
The choice of treatment for liver cirrhosis depends on several factors, including the stage and severity of the disease, the underlying cause, the patient’s overall health, and their preferences. It’s important to work closely with a healthcare professional to determine the most appropriate treatment plan and monitor progress over time.
Complications
Liver cirrhosis can lead to a range of serious complications that significantly impact patient outcomes and quality of life.
These complications include:
- Portal hypertension
- Hepatic encephalopathy
- Hepatocellular carcinoma
Portal Hypertension
Portal hypertension refers to increased pressure in the portal vein, which carries blood from the intestines and spleen to the liver. In cirrhosis, the damaged liver tissue obstructs the flow of blood, leading to a buildup of pressure in the portal vein.
This increased pressure can cause:
- Esophageal varices: Enlarged veins in the esophagus that can rupture and bleed
- Ascites: Accumulation of fluid in the abdomen
- Splenomegaly: Enlargement of the spleen
Hepatic Encephalopathy
Hepatic encephalopathy is a condition that occurs when the liver is unable to remove toxins from the blood, leading to a buildup of these toxins in the brain.
Symptoms of hepatic encephalopathy can range from mild to severe and may include:
- Confusion and disorientation
- Personality changes
- Tremors
- Coma
Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) is a type of liver cancer that is often associated with cirrhosis. In cirrhosis, the damaged liver cells are more likely to undergo malignant transformation, leading to the development of HCC.
HCC is a serious condition that can be difficult to treat, and it is a leading cause of death in patients with cirrhosis.
Prognosis
The prognosis of liver cirrhosis depends on several factors, including the severity of the disease, the underlying cause, and the patient’s overall health. Without proper treatment, liver cirrhosis can lead to serious complications, such as liver failure, portal hypertension, and hepatocellular carcinoma.
The 5-year survival rate for patients with compensated cirrhosis is around 70-80%. However, the survival rate drops to 50% or less for patients with decompensated cirrhosis. The presence of complications, such as ascites, encephalopathy, or variceal bleeding, further worsens the prognosis.
Patient Education and Adherence to Treatment Plans
Patient education and adherence to treatment plans are crucial for improving the prognosis of liver cirrhosis. Patients need to understand the disease, its complications, and the importance of following their treatment plan. This includes:
- Avoiding alcohol consumption
- Maintaining a healthy diet
- Taking medications as prescribed
- Getting regular check-ups
By following their treatment plan, patients can help to slow the progression of liver cirrhosis, reduce the risk of complications, and improve their overall survival.
Case Study
A 55-year-old male patient presented with a history of heavy alcohol consumption for over 20 years. He had no significant past medical history. Over the past few months, he had experienced progressive fatigue, abdominal pain, and swelling in his legs.
On physical examination, he was jaundiced with spider angiomata and palmar erythema. His abdomen was distended with ascites, and his liver was palpable 4 cm below the right costal margin. His spleen was also palpable.
Laboratory results showed elevated liver enzymes (AST 150 U/L, ALT 120 U/L), hyperbilirubinemia (total bilirubin 3.0 mg/dL, direct bilirubin 2.0 mg/dL), and hypoalbuminemia (2.5 g/dL). A liver biopsy confirmed the diagnosis of cirrhosis.
The patient was treated with diuretics for ascites, lactulose for hepatic encephalopathy, and vitamin K for coagulopathy. He was also advised to abstain from alcohol. Despite treatment, his condition worsened, and he developed hepatorenal syndrome and died from liver failure 6 months after the diagnosis of cirrhosis.
Conclusion
Liver cirrhosis is a severe and potentially life-threatening condition that can lead to a range of complications. Early diagnosis and appropriate management are crucial for improving patient outcomes and preventing complications.
Patient education plays a vital role in managing liver cirrhosis. Patients need to be aware of the condition, its causes, and the importance of adhering to treatment plans. They should also be informed about the potential complications and the signs and symptoms to watch out for.
Implications for Clinical Practice, Case study about liver cirrhosis
- Clinicians should be vigilant in screening and diagnosing liver cirrhosis, especially in patients with risk factors such as chronic hepatitis, alcohol abuse, or non-alcoholic fatty liver disease.
- Early diagnosis allows for prompt initiation of treatment, which can help slow the progression of the disease and prevent complications.
- Patient education is an essential component of managing liver cirrhosis. Patients need to be empowered with knowledge about their condition and its management.
- Close monitoring and follow-up are crucial for patients with liver cirrhosis to assess the progression of the disease, identify and manage complications, and adjust treatment plans as needed.
User Queries
What are the common causes of liver cirrhosis?
Alcohol abuse, viral hepatitis (hepatitis B and C), non-alcoholic fatty liver disease (NAFLD), autoimmune disorders, and genetic conditions.
What are the early signs and symptoms of liver cirrhosis?
Fatigue, loss of appetite, nausea, abdominal pain, and swelling in the legs or ankles.
What is the treatment for liver cirrhosis?
Treatment options vary depending on the stage of cirrhosis and may include medications, lifestyle modifications, and surgical interventions such as liver transplantation.